Legal Framework for Hospitals in India: Healthcare Licenses, Regulations, and Compliance
Starting and running a hospital in India is a real challenge beyond medicine. It involves filtering through a dense blanket of legal frameworks, obtaining a barrage of healthcare licenses and permits and ensuring continued compliance with a mountain of regulations. Thus, failing to fulfill these regulatory commitments can lead to serious consequences like substantial fees, the loss or suspension of the license offered to a professional, and even criminal allegations in some situations.
This blog covers the legal aspects of running a hospital in India, and how to get healthcare licenses, regulations & compliances to run a hospital in India. Requirements that you must adhere to to run a hospital in India.
Basic Healthcare Licenses and Registrations
Even before its doors can open, a hospital must obtain a dozen foundational healthcare licenses and registrations from the government.
They further need to comply with the registration under the Clinical Establishments (Registration and Regulation) Act, 2010 (CEA). This is the central legislation that governs the establishment and regulation of clinical establishments, including hospitals across the country.
The objective of the act is to ensure the standardisation of healthcare facilities and the quality of healthcare services, ensure minimal levels of quality and safety, and improve accessibility and affordability of services.
The CEA applies in those states and union territories that have adopted it. States are free to enact their own clinical establishment acts that might have similar or additional requirements.
Procedure for Registration for Healthcare Licenses
Hospitals shall apply to the concerned registering authority (generally at the state level) with detailed particulars of the infrastructure, facilities, services, and personnel available. Before approving healthcare licenses, the competent authority performs on-site inspections to confirm compliance with adequate standards.
Further, hospitals can be classified by various criteria, such as size, degree of specialisation, or range of services, with each category subject to different requirements. Getting healthcare licenses under the CEA is generally valid for a limited time, and therefore, periodic renewal is required.
Business Registration and Incorporation
As per the ownership structure (private limited company, public limited company, trust, society, etc.), the hospital must be registered and incorporated under the relevant laws, such as the Companies Act, 2013, or the other relevant state-level acts, if it is a trust or society. This allows the hospital entity to be legally recognised and obtain all the necessary healthcare licenses.
GST Registration
Many hospitals providing services (beyond true charitable work, which attracts certain exemptions) are required to obtain GST registration and adhere to invoicing, tax collection and return filing provisions.
Trade Licenses
To run the hospital in their jurisdiction, trade healthcare licenses must be obtained from the local municipal authorities. This healthcare license confirms that commercial activity is being conducted on the premises in question.
Infrastructure & Safety Regulations
Hospitals are subjected to strict regulations regarding their infrastructure, construction safety and environmental compliance.
Compliance with Building By-laws and Fire Safety
The building by-laws of the local municipal corporation or development authority govern hospitals. Importantly, they must also comply with fire safety regulations, including adding systems for detection and suppression of fire, adding fire exits, and conducting regular fire safety audits.
Biomedical Waste Management Rules, 2016
Hospitals generate a lot of biomedical waste, which, if not managed properly, can cause environmental and health hazards. These rules are provided for the segregation, collection, storage, transportation, treatment, and disposal of various categories of biomedical waste. Hospitals are required to have effective waste management, undertake training, and document waste disposal.
Water and air pollution control regulations
Domestic hospitals must comply with regulations aimed at controlling water and air pollution. This may include obtaining discharge permits for effluents and emissions, establishing effluent treatment systems, and meeting prescribed standards.
Regulations on Radiation Safety
If a hospital has a department of radiology or a nuclear medicine facility. In that case, it shall comply with Atomic Energy (Radiation Protection) Rules, 2004 and other rules that may be relevant to ensure the safe handling, storage, and disposal of radioactive substances and the protection of the patients, staff and general public against radiation hazards. This includes securing healthcare licenses from the Atomic Energy Regulatory Board (AERB) and establishing stringent safety measures.
Operational and Clinical Regulations
In addition to infrastructure, hospitals are governed by a host of regulations concerning their daily operations and clinical practices.
Medical Council of India (MCI) / National Medical Commission (NMC): These are standards set by the aforementioned bodies which include standards of medical education, professional conduct, and ethical practices. In the case of hospitals that employ their own doctors, they must ensure that the medical staff are registered with the relevant medical council and also that they comply with these regulations. The MCI has now been dissolved and the NMC Act, 2019, replacing it, is being gradually brought into force.
Indian Nursing Council (INC) And State Nursing Council Regulations : Likewise, the INC and state nursing councils are responsible for regulating the education and practice of nurses. Nurse registration and meeting professional standards are the responsibility of the hospitals employing them.
Drugs and Cosmetics Act, 1940, and Rules, 1945: Hospitals with in-house pharmacies or dispensing units are required to comply with the provisions of this act and its rules related to storage, dispensing, and labeling of drugs. They might need certain permits for their pharmacies.
Indian Laws on Organ Donation to Prevent Organ Trafficking: The Transplantation of Human Organs and Tissues Act of 1994 is a strict act under which only registered hospitals are involved in organ transplantation.
Pre-conception and Pre-natal Diagnostic Techniques (Prohibition of Sex Selection) Act, 1994: Hospitals and clinics providing ultrasound or other pre-natal diagnostic procedures must ensure adherence to the provisions of this act, which prohibits the determination of sex. These requirements include keeping a written record of the use of automated decision systems (Form F), posting the requisite signage, and complying with restrictions on these technologies.
Mental Healthcare Act, 2017: This act applies to mental healthcare services provided by hospitals and is intended to protect the rights of persons with mental illness and regulate the provision of mental healthcare.
National Accreditation Board for Hospitals & Healthcare Providers (NABH) Standards: Although not legally inescapable, NABH standards are voluntary for hospitals and healthcare Providers and validate/promote identical superior quality and patient safety. Numerous hospitals aim for NABH accreditation in an effort to build their credibility and draw patients. They often meet regulatory standards by complying with NABH standards.
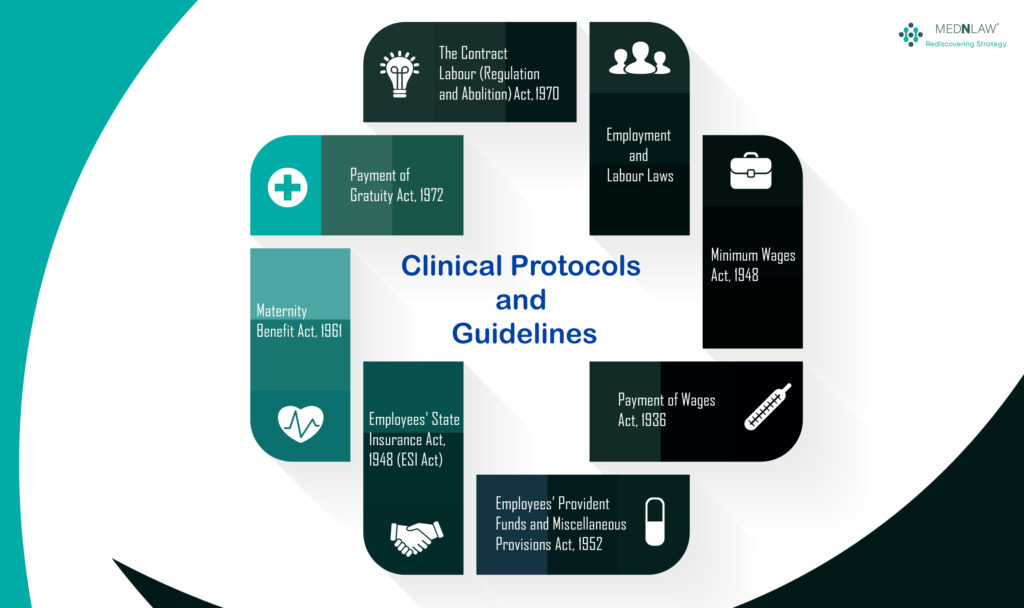
Clinical Protocols and Guidelines
Hospitals should adhere to evidence-based clinical protocols and guidelines for the diagnosis and treatment of various medical conditions. These guidelines are vital for the provision of adequate care and the prevention of medical malpractice.
Employment and Labour Laws: Hospitals are not only commercial establishments, but they are also employers, and therefore, they are subject to several labour laws in India:
Minimum Wages Act, 1948: The act ensures that minimum wages set by the government are paid to the employees.
Payment of Wages Act, 1936: The act regulates the time frame for the payment of wages and unauthorised deductions.
Employees’ Provident Funds and Miscellaneous Provisions Act, 1952: The act has provisions for the establishment of provident funds for employees and offers benefits.
Employees’ State Insurance Act, 1948 (ESI Act): The act provides medical and other benefits to employees in the healthcare sector.
Maternity Benefit Act, 1961: The act grants maternity leave and benefits to pregnant women employees.
Sexual Harassment of Women at Workplace (Prevention, Prohibition and Redressal) Act, 2013 (POSH Act): The act aims to prevent and redress sexual harassment in the workplace to ensure a safe working environment for women.
Payment of Gratuity Act, 1972: Under the Payment of Gratuity Act of 1972, employers pay a lump sum to their employees as a retirement benefit upon completion of 5 years of continuous service or upon death or disablement.
The Contract Labour (Regulation and Abolition) Act, 1970: The Contract Labour (Regulation and Abolition) Act of 1970 seeks to regulate the employment of contract labour in certain establishments and provides for its abolition 2 in certain circumstances to prevent exploitation and secure welfare.
Data Privacy and Security
Data privacy and security are top priorities with the increasing digitisation of health care records.
Information Technology Act, 2000: Even though now there is a specific data protection law applicable (Digital Personal Data Protection Act, 2023), these laws and rules (related to sensitive personal data and, at times, data security) shall still hold ground, given the new act is not implemented fully.
Undertaking the security of data within healthcare sectors, hospitals carrying patient data electronically must follow reasonable security practices and procedures to protect patient data.
Compliance and Enforcement
Maintaining compliance with all existing legislation and regulations is necessary for hospitals to function correctly and legally. This involves:
Policies, Procedures and Internal Audits: It creates and enforces internal compliance mechanisms to maintain compliance and ensure adherence to legal mechanisms.
Routine Staff Training: Keeping all hospital staff updated on the laws, rules and internal policies that are relevant makes them more efficient and
Well-maintained records: Keeping detailed and up-to-date records as mandated by multiple laws is mandatory and can also act as proof in case of any medical negligence suit.
Inspections and Audit: Responding to all inspections and audits performed by various regulatory bodies also contributes to efficiency and accountability.
Timely Corrective Action: Implementing corrective action immediately to respond to such identified instances of non-compliance.
Different authorities from the central, state, and local levels all enforce these laws. Non-compliance can result in:
- Fines and Penalties: There are monetary penalties for transgressions against particular sections.
- Healthcare Licenses Suspended or Revoked: Their operation healthcare licenses can be temporarily or permanently revoked if non-compliance is proven.
- Legal Prosecution: Criminal prosecution for serious violations like sex determination for money or negligence cause harm to a patient. Thus, there are provisions under the IPC and BNS, along with acts like PCPNDT, to combat it.
- Loss of Public Trust: Medical negligence suits against a specific hospital not only result in the revoking of healthcare licenses and criminal charges but also result in Negative publicity and reputational damage.
Conclusion:
Running a hospital in India is a legally complex business that requires painstaking attention to hundreds of healthcare licenses, regulations and compliance requirements. From essential registrations to complex clinical and safety protocols, healthcare providers like you must navigate this complex structure carefully to keep your patients healthy, your staff safe, and your hospital legally safe. It’s not only about meeting legal regulations, but proactive compliance, strong internal processes, and ethical practices are the foundation for building a trustworthy and sustainable healthcare organisation in India.
The legal framework is dynamic and remains so. Knowledgeable, specialised legal counsel is paramount to the ever-changing, effective navigation of this maze and the provision of quality healthcare within the sands of the law.
-
 Overview of the Clinical Establishments Act of 2010 in India9:58 am GMT+00:00•April 28, 2025Read more
Overview of the Clinical Establishments Act of 2010 in India9:58 am GMT+00:00•April 28, 2025Read more -

-

Here are some related articles you may find interesting
Copyright Mednlaw