Informed Consent is the foundation of the doctor-patient relationship. It informs the patients about the potential risks, benefits and any alternatives of the proposed medical treatment. Informed Consent is not just a legal requirement but also an ethical imperative, empowering patients to make informed decisions about their own healthcare.
Furthermore, from a medico’s perspective obtaining informed Consent involves more than just having a patient sign a form. It is a process that requires effective communication from both the ends, and a deep understanding of the patient’s needs and concerns.
As a healthcare provider, the role of a doctor in obtaining informed consent is important not only from legal and ethical points of view but also to maintain trust, a doctor-patient relationship, and to ensure patient-centered care. This article discusses informed consent from a doctor’s point of view, its importance, the ethical and legal responsibilities of doctors, and how the informed consent process can be enhanced for better patient outcomes.
Key Elements of Informed Consent
Informed consent is basically based on four principles: autonomy, beneficence, non-maleficence, and justice, which can guide ethical practice in medicine. Autonomy refers to the right of the patient to decide over his body and health care, in line with the values, beliefs, or preferences he holds.
Respect for autonomy is implied in the context of informed consent, putting the patient in a position of having to make a decision that is free from any compulsion and undue influence.
It is essential that informed Consent is obtained effectively. There are several key elements that must be addressed; they are mentioned below:
Disclosure of Information:
The Doctor’s must provide patients with all relevant information regarding the treatment, which includes the purpose, potential risks, and benefits, alternative treatments and the potential consequences of refusing the treatment.
Understanding by the patient:
It is very crucial for the doctors to ensure that the patients understand the information provided. The process may involve using clear and simple language, avoiding medical terminology and answering all the questions that the patient may have.
-
- Use of Simple Language – Use of simple language and avoiding the use of medical terminology will help the patients have an understanding of the process and steps related to it.
- Check for comprehension – It is integral for the doctor to ask the patient to explain the information in their own words to ensure understanding.
- Using Visual Aids – Use of diagrams, models or other visual aids help the patient and their families to have a better understanding of the treatment process, its benefits and risks related to it.
- Addressing questions and concerns – Directing the concern and questions related to the process, will bring a better understanding to the patient.
Voluntariness:
It is integral for the patient to be free from coercion or undue influence when making their decision. Also, doctors should not pressure patients to undergo a particular treatment.
Competence:
While making the decision the patient must be in the mental capacity to understand the information provided and make a reasoned decision. If a patient’s capability to make decisions is impaired because of medical factors like dementia, mental illness or intoxication, the doctor shall seek guidance from a legal or ethical advisor. The medico may also consult the family of the patient.
Challenges in Obtaining Informed Consent :
The fundamental principle for obtaining informed Consent is medical ethics. However, sometimes it is challenging in practice, let’s know more about these challenges:
Time Constraints
Life of a medico is usually busy, thus it can be tough to allocate sufficient time for detailed conversations about the treatment. Medical terminology is tricky, thus explaining complex medical information to the patients with limited language proficiency can be challenging.
Cultural Differences
Cultural differences and beliefs influence the patient’s decision making. It may also affect the patient’s decision making and their understanding of risk and benefit. In such a situation healthcare professionals can consult the patient’s family or a legal and ethical advisor.
Patient Anxiety
Most of the time, it is seen that the patient is distressed or anxious, which can make it difficult for them to understand and process information fully.
Technological Advancements
The rapid advancements in healthcare technology makes it challenging for the doctors to keep up with the latest information and communicate effectively to patients.
Cognitive Impairments
Obtaining a consent from patient who has cognitive impairments, like dementia or mental illness might not be able to provide with informed consent. In such situations it is important for the healthcare professional to take informed consent from the patient’s family or they can also consult an ethical and legal advisor.
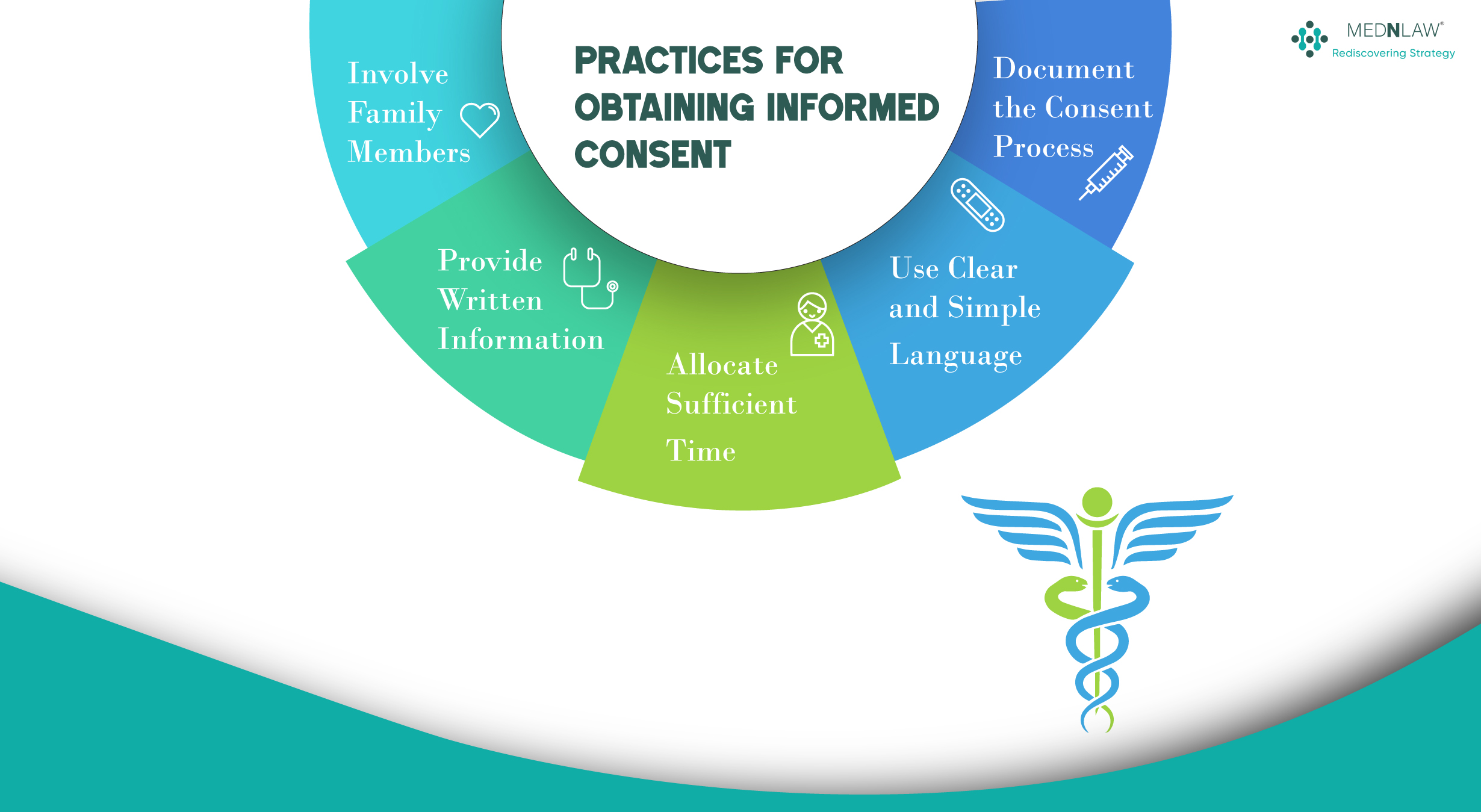
Practices for Obtaining Informed Consent
It is very important for the doctors to overcome the above mentioned challenges in order to safeguard their practice. The healthcare professional can follow mentioned practices to protect their practices from medical negligence suits.
Allocate Sufficient Time
A medico has to allocate some time with their patient in order to explain the treatment process, its benefits, risks and other treatment options. Further, it is equally integral to clear all the doubts and queries of the patients thoroughly.
Use Clear and Simple Language
It is very important for healthcare professionals to avoid medical jargon, instead the use of plain and simple language would be preferred as it could be understood by patients.
Provide Written Information
While explaining the process and other related topics it is very important to provide written materials, such as brochures or pamphlets.
Involve Family Members
Involving family members or caregivers is equally vital in the decision-making process.
Document the Consent Process
This is the most essential process of all. Maintaining a clear and accurate documentation of the informed Consent is integral. Further, the information provided to the patient, the patient’s question and concerns should be mentioned in the informed Consent along with the patient’s decision.
Following these practices and further prioritising patients’ understanding, doctors can ensure that informed Consent is a meaningful and valuable part of the treatment process.
Legal Dimensions of Informed Consent
In terms of legal consideration, consent is a core right of a patient, while the failure of obtaining proper consent often leads to liabilities against the physician. Medical malpractice, including the specific notion of battery (untoward touching or procedures), follows the failure in obtaining informed consent. In numerous jurisdictions, malpractice or injury suits may occur because of such a failure of informed consent.
For instance, Indian law provides that informed consent is a prerequisite for medical interventions. The Medical Council of India, under the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002, clearly mandates that a doctor must inform patients regarding the diagnosis, proposed treatment, risks, and benefits of the procedure. Similarly, cases like Samira Kohli v. Dr. Prabha Manchanda (2008) and Poonam Verma v. Ashwin Patel (1996) has established that medical professionals must ensure patients are adequately informed before any medical intervention, and consent must be obtained in writing for procedures with significant risks.
Informed consent also involves ensuring that the patient has the capacity to understand the information provided. This capacity can be influenced by factors like age, the status of a patient’s mental health, and language barriers. As a doctor, he should ensure that the patient is able to understand the information being given to him. If there are concerns about the patient’s ability to understand the details, such as minors or individuals with cognitive impairments, alternative methods, such as involving a legal guardian or translator, may be necessary.
Landmark Cases Related to Informed Consent
Landmark cases introduced the concept of informed consent in India and establish its importance in protection of patients’ rights and understanding of medical ethics. The following is a selection of the most important landmark cases which have shaped the law of informed consent in India:
Dr Thomas v Smt. Elisa
In this case, the apex court ruled that the doctor was negligent for not operating on the patient with a life threatening condition because the patient could not provide consent.
Paramanand Katara Vs the Union of India
The supreme court ruled that the doctors have an ethical and legal duty to treat the patients who are in life-threatening situations, even without their consent.
Samira Kohli v. Dr. Prabha Manchanda (2008)
This is one of the prominent cases which deals with informed consent in medical procedures. Here, the apex court ruled that the patient’s right to informed consent is paramount. Thus, the judgement clarified that informed consent is not just a formality but a process that requires the patient to be fully informed of the procedure.
Importance of Informed Consent
Informed Consent is an integral component of ethical and quality healthcare. Further, understanding the principles of informed Consent and adopting the best practices will always maintain a good doctor-patient relationship, decreasing the chances of getting a medical negligence suit.
Furthermore, informed Consent is not just a legal requirement. Instead, it’s an ethical and rudimentary pillar for building strong relationships with patients. When the patients feel informed and empowered to make decisions about their health and treatment process, they are more likely to stick to the treatment plan and take accountability if needed. This also increases the trust of patients towards the doctor and experience more effective health outcomes.
-
 Overview of the Clinical Establishments Act of 2010 in India9:20 am GMT+00:00•April 28, 2025Read more
Overview of the Clinical Establishments Act of 2010 in India9:20 am GMT+00:00•April 28, 2025Read more -

-

Here are some related articles you may find interesting
Copyright Mednlaw